Whether you’re reconsidering your current approach to contraception or starting birth control for the first time, you have options. Some are available over the counter, while others require a doctor’s visit.
There are four types of birth control: lifestyle or behavioral changes, methods you use only as needed, contraceptives you take on a consistent schedule, and surgical sterilization.
As you explore your options, you might find it helpful to consider the following questions:
- What level of pregnancy risk are you comfortable with?
- Do you want your birth control to reduce sexually transmitted infection (STI) transmission risk too?
- How do you feel about receiving a pelvic exam?
- Can you realistically use something on a set schedule?
- Are you trying to manage hormonal acne or other symptoms?
- Do you want children in the future? How about the near future?
- What’s your budget?
It’s a great idea to make an appointment with a healthcare professional to discuss your answers to these questions and more. They can help address any concerns you might have.
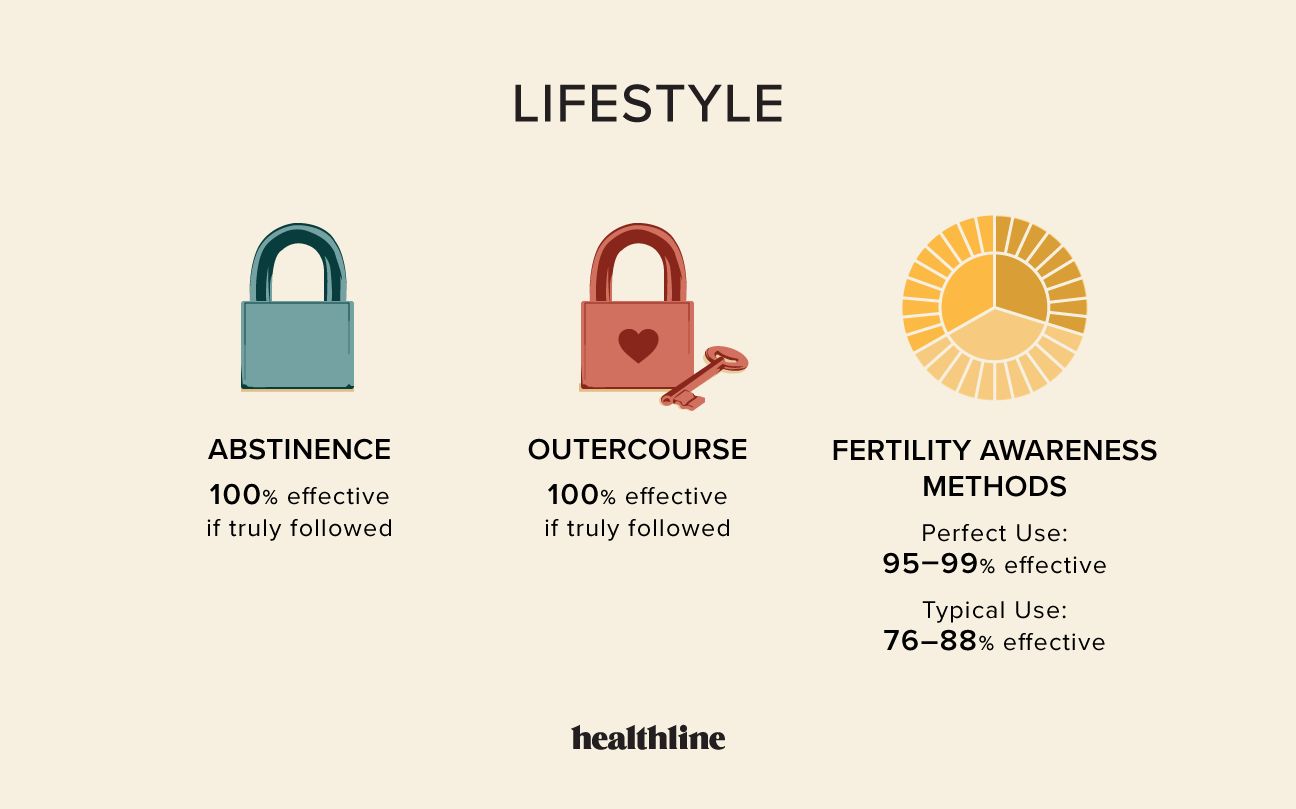
Abstinence
“Abstinence means something different to everyone,” says Felice Gersh, MD, author of “PCOS SOS: A Gynecologist’s Lifeline to Naturally Restore Your Rhythms, Hormones and Happiness.”
If you want to prevent pregnancy, it means specifically avoiding penis-in-vagina (P-in-V) penetration.
“It’s incredibly effective for folks who are actually committed to never having intercourse,” adds Gersh.
Outercourse
“Outercourse” is definition-wiggly. For some, outercourse means no vaginal or anal penetration of any kind, including fingers and sex toys.
The effectiveness rate of outercourse will depend on how you and your partner(s) define it. If you choose to avoid any type of P-in-V sex, it has a 100% effectiveness rate.
Fertility awareness methods
These methods involve tracking your menstrual cycle and other bodily changes so that you can avoid P-in-V sex during your fertile window.
You can use the following tracking methods:
- the calendar method, which involves tracking the timing of your cycle over several months
- the temperature method, which helps you estimate ovulation by tracking temperature changes
- the cervical mucus method, which involves tracking changes in vaginal discharge
Although fertility awareness methods can be a great way to learn more about your body, they have a high failure rate when used as contraception.
“Usually, fertility awareness methods are a far better route if you are actively trying to become pregnant,” says Dr. G. Thomas Ruiz, an OB-GYN at MemorialCare Orange Coast Medical Center in Fountain Valley, California.
According to the American College of Obstetricians and Gynecologists, fertility awareness methods are 76% to 88% effective in the first year of “typical use,” which accounts for human error. With perfect use, they’re 95% to more than 99% effective.
External condom
An external condom covers your penis and is designed to catch any fluid that comes out, including pre-ejaculate.
- Effectiveness: perfect use: 98%; typical use: 87%
- Average cost: up to $2 each
- Pros: External condoms help prevent STIs. Latex and latex-free options are widely available.
- Cons: They’re not foolproof. Although some people say that condoms boost pleasure, those who are used to barrier-free sex may find the opposite.
Internal condom
An internal condom is a polyurethane pouch that you insert into your vagina.
- Effectiveness: perfect use: 95%; typical use: 79%
- Average cost: up to $2 to $3 each
- Pros: Internal condoms are latex-free, help protect against STIs, and can be inserted up to 8 hours in advance. Some people enjoy that they feel less snug around the penis than external condoms.
- Cons: Internal condoms have a bit of a learning curve. They aren’t hard to use, necessarily, but they do take some practice.
Diaphragm
The diaphragm is a soft silicone disk. You saturate it with spermicide and then insert it into your vaginal canal, where it covers your cervix.
- Effectiveness: perfect use: 94%; typical use: 83%
- Average cost: up to $75, plus the cost of the doctor’s visit and the cost of the spermicide
- Pros: This method can be used for up to 24 hours at a time as long as you add spermicide every 6 hours. A diaphragm is reusable, so be sure to clean it thoroughly and store it somewhere sterile.
- Cons: A diaphragm requires a prescription and can get knocked out of place with aggressive thrusting. And it’s not a great option for folks who are prone to urinary tract infections.
Sponge
The sponge is actually a plastic disk saturated with spermicide. You insert it deep inside your vaginal canal, where it covers your cervix and blocks sperm from entering your uterus.
- Effectiveness: perfect use: 91% if you’ve never given birth, 80% if you have; typical use: 86% if you’ve never given birth, 78% if you have
- Average cost: up to $15 for 3, plus the cost of the spermicide
- Pros: You can insert it up to 24 hours in advance and use it for up to 24 hours after insertion.
- Cons: You have to leave the sponge in place for 6 hours after P-in-V sex, which some folks say feels messy. There’s also a slightly increased risk of toxic shock syndrome.
Cervical cap
A cervical cap is a soft silicone cup. You fill it with spermicide and then insert it deep into your vaginal canal, where it covers your cervix.
- Effectiveness: if you’ve never given birth: 86%; If you have given birth: 71%
- Average cost: up to $90, plus the cost of the doctor’s visit and the cost of the spermicide
- Pros: The cap can be used for up to 48 hours at a time, and you don’t have to reapply spermicide. It’s reusable with proper care.
- Cons: The cap has to be left in place for 4 hours after P-in-V sex, which some find bothersome. It requires a prescription and must be replaced every 12 months.
Spermicide
Spermicide can be used by itself. Squirt or insert the substance into your vaginal canal before P-in-V sex.
- Effectiveness: perfect use: 86%; typical use: 79%
- Average cost: up to $270, depending on the form and brand
- Pros: Spermicide gel is available over the counter at many drugstores.
- Cons: It takes 10 to 15 minutes to dissolve before you can engage in vaginal penetration. It must be reapplied after an hour of use.
Emergency contraceptive pills ≠ birth controlPlan B, ella, and other emergency contraceptive pills are highly effective when taken within 3 to 5 days of sex without a barrier. But it’s important to avoid using them as routine contraception.
“It’s an effective fallback, but it’s nowhere near as effective as the birth control options,” Ruiz says. Plus, “It’s a very high dose of hormones, so taking it regularly probably won’t make you feel very good.”
Shot
The shot uses the hormone progestin to prevent ovulation. It must be given by a healthcare professional every 90 days.
- Effectiveness: perfect use: over 99%; typical use: 96%
- Average cost: up to $150 per shot, plus the cost of the doctor’s visit
- Pros: It’s super effective if you can get to an appointment every 12 to 13 weeks. Many users report that the shot lessens period-like bleeding or stops it altogether.
- Cons: Nausea, headaches, dizziness, weight gain, and depression have been reported. If you later decide to try to become pregnant, know that it could take up to a year after your last dose for your fertility to return.
Ring
Available by prescription only, the plastic ring uses estrogen and progestin to prevent ovulation. You insert the ring deep into your vaginal canal for up to 3 weeks of protection and then remove it for 1 week to have period-like bleeding.
- Effectiveness: perfect use: 99%; typical use: 93%
- Average cost: up to $200 per ring, plus the cost of the initial doctor’s visit
- Pros: Many people report that it helps with acne and makes period-like bleeding more regular.
- Cons: Chest tenderness and headaches are the most commonly reported side effects. Although you should be protected from pregnancy the week you aren’t wearing a ring, pregnancy is a risk if you’re off schedule.
Patch
The prescription patch releases estrogen and progestin into your body to stop ovulation. You apply a new patch to your upper arm, butt, or back every week for 3 weeks and then skip a week so you can have period-like bleeding.
- Effectiveness: perfect use: 99%; typical use: 93%
- Average cost: up to $150 per month, plus the cost of the initial doctor’s visit
- Pros: Many users report no side effects.
- Cons: It requires weekly diligence, which means there’s a high risk of human error. When side effects are reported, they include nausea, headaches, chest tenderness, and skin irritation.
Combination pill
The combination pill uses estrogen and progestin to prevent your ovary from releasing an egg. It must be taken at roughly the same time each day to work.
- Effectiveness: perfect use: 99%; typical use: 93%
- Average cost: up to $50 per pack, plus the cost of the initial doctor’s visit
- Pros: It can help reduce the severity of menstrual symptoms.
- Cons: The combination pill is available by prescription only. Forget to take it, and the effectiveness goes way down. In other words, the risk of human error is high.
Minipill
Also known as the progestin-only pill, the minipill is a great pick for folks who wish to avoid estrogen.
- Effectiveness: perfect use: 99%; typical use: 93%
- Average cost: up to $50 per pack, plus the cost of the initial doctor’s visit for most pills
- Pros: The minipill can help reduce the severity of menstrual symptoms. Although most minipills require a prescription, you can get Opill over the counter at your local pharmacy or purchase it online.
- Cons: Some people report chest tenderness and acne flare-ups. Like the combination pill, the minipill must be taken at roughly the same time every day to be effective.
Implant
The implant is a plastic rod about the size of a matchstick that releases progestin into your body. A healthcare professional will place it under the skin of your arm.
- Effectiveness: over 99%
- Average cost: up to $2,300 for the device and initial appointment, plus the cost of any follow-up visits and eventual removal
- Pros: The implant lasts up to 5 years and can be removed at any time. “A major perk is that it doesn’t require a pelvic exam, which is why it’s the option most used by younger menstruators,” Ruiz says.
- Cons: Insertion requires local anesthetic and a big-ish needle, and you may be sore for a few days afterward. It can cause irregular bleeding, acne, chest tenderness, and weight gain.
Copper intrauterine device (IUD)
An IUD is a small, T-shaped instrument that a healthcare professional inserts through your vaginal canal into your uterus. Copper IUDs, sometimes called nonhormonal IUDs, work by repelling sperm.
- Effectiveness: over 99%
- Average cost: up to $1,800 for the device and initial appointment, plus the cost of any follow-up visits and eventual removal
- Pros: The copper IUD lasts up to 12 years and can be removed at any time. If you decide you want to get pregnant, you can start trying immediately after removal. “You also still get a period every month, which some menstruators find comforting,” Ruiz notes.
- Cons: Side effects include spotting between periods, increased menstrual cramps, and heavier menstrual bleeding. Many people experience pain or discomfort during or after the insertion process.
Hormonal IUD
A hormonal IUD uses progestin to prevent ovulation. A healthcare professional inserts the device into your uterus.
- Effectiveness: over 99%
- Average cost: up to $1,800 for the device and initial appointment, plus the cost of any follow-up visits and eventual removal
- Pros: Depending on the brand, the hormonal IUD is effective for 3 to 8 years. It can also be removed at any time. “The progestin only circulates in the genital region and is much, much lower than the amount found in [the] pill,” adds Ruiz.
- Cons: Possible side effects include spotting between periods, cramping, and irregular period-like bleeding. Many people experience pain or discomfort during or after insertion.
Vasectomy
Vasectomy involves blocking or cutting the tubes that carry sperm from your testicles to your penis. This prevents sperm from being added to ejaculate.
- Effectiveness: over 99%
- Average cost: up to $1,000, plus the cost of any follow-up visits
- Pros: While a vasectomy can be reversed in some cases, it’s considered permanent. It’s an outpatient surgery, meaning you can usually go home the same day.
- Cons: It takes a few months for your ejaculate to be sperm-free, so you’ll need to use a condom or other birth control method until your healthcare professional confirms the surgery was successful.
Tubal ligation
Tubal ligation involves blocking, tying, or cutting your fallopian tubes to prevent an egg from reaching your uterus.
- Effectiveness: over 99%
- Average cost: up to $6,000, plus the cost of any follow-up visits
- Pros: While it may be possible to reverse the results or get pregnant via in vitro fertilization, tubal ligation is considered permanent. It’s an outpatient surgery.
- Cons: You may experience pain and discomfort during recovery.
“There’s a common misconception that people assigned female at birth who are taking testosterone can’t get pregnant, but that’s not always true,” says trauma-focused clinician and sexuality educator Aida Manduley, LICSW.
“Unless a medical provider has told you you’re sterile or unable to get pregnant, assume pregnancy is a risk,” Manduley says.
In other words, depending on the anatomy of your partner and the type of sex you’re having, you may want to look into birth control. Gender affirming hormone therapy and hormonal birth control can be safely used together.
Optum Perks is owned by RVO Health. By clicking on this link, we may receive a commission. Learn more.
| Symptom | Best birth control option |
|---|---|
| hormonal acne | combination pill |
| gender dysphoria | implant |
| heavy period | hormonal IUD |
| polycystic ovary syndrome | combination pill |
| menstrual cramps | combination pill |
The kitschy line “Smile baby, you’re alive. You’ve got options” is apt here. It just comes down to your individual lifestyle and priorities. And remember, you don’t have to figure it out all on your own — a doctor can help.










