In multiple sclerosis (MS), the body attacks myelin, the protective coating of nerves in the brain. This leads to various symptoms, such as memory issues, fatigue, lack of concentration, slow processing speed, and mood changes.
MS is an unpredictable and long lasting disease of the central nervous system causing a block of nerve messages in the brain and spinal cord.
Here’s an in-depth look at how MS affects the brain.
Cognitive dysfunction, also called impaired thinking, is a neurological problem that affects more than half of people with MS, according to a
Cognition refers to high-level functions carried out by the brain, including:
- memory
- planning
- problem-solving
- processing information
- verbal fluency or finding words
- visual perception
- attention
Most people with MS who experience cognitive dysfunction will have mild to moderate problems that may only involve one or two areas. Memory issues such as acquiring, retaining, and retrieving new information are the most frequently reported cognitive challenges.
Concentration problems are another potential type of cognitive dysfunction, specifically when it comes to paying attention and multitasking.
The National MS Society stresses the importance of early recognition of cognitive changes but also recognizes how subtle these changes may be, especially at first.
Some common early signs may include having difficulty:
- finding the right words
- remembering what to do in your job or during daily routines
- keeping up with tasks or conversations
Does MS affect decision-making?
MS can affect your decision-making ability. While the degree can vary from person to person, one
MS mainly affects the white matter in the brain stem, cerebral cortex, optic nerve, and spinal cord. However, it can also affect gray matter, especially when the disease is very advanced.
Generally, MS affects the brain in the following order:
- Inflammation: An autoimmune attack releases white blood cells that cause changes to neurons in the brain and spinal cord.
- Inflammatory demyelination: A nerve fiber, known as an axon, is a thin strand of brain neuron that travels from the cell body and sends signals to other cells. This is what allows you to talk and move.
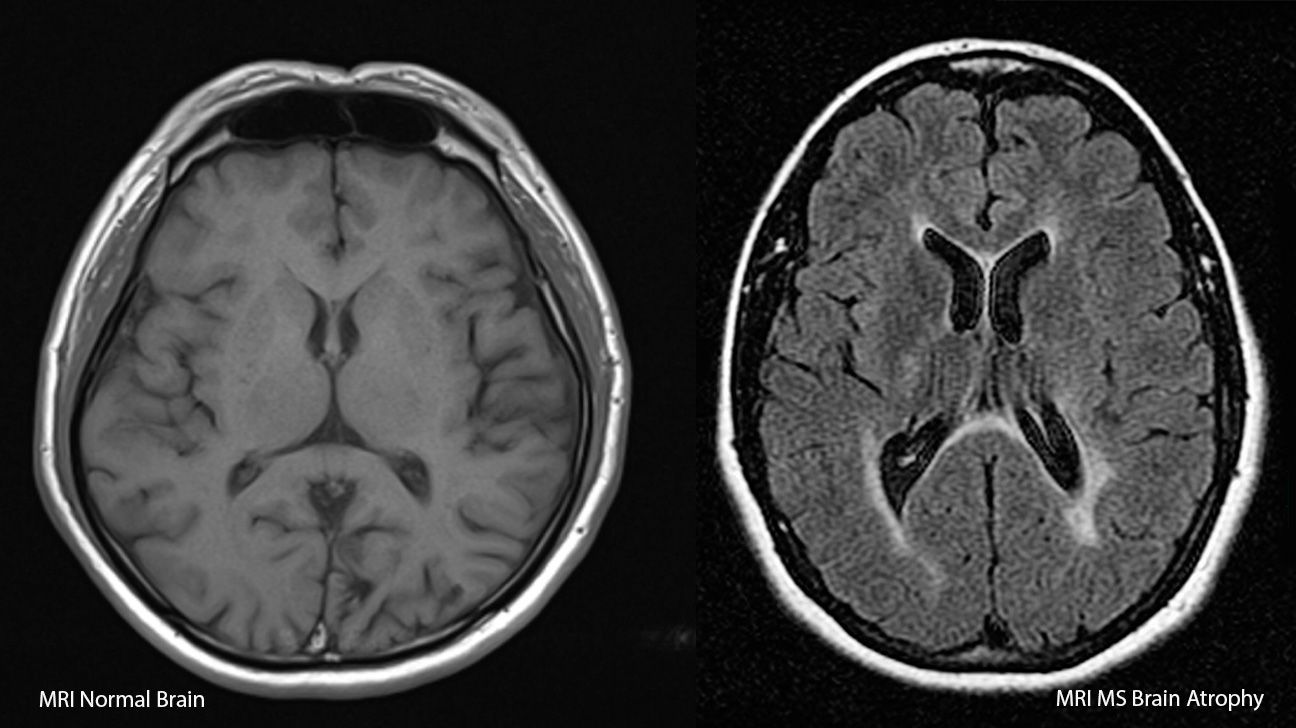
Myelin acts as a protective coating around the nerves, but if it’s damaged, the fibers struggle to send their messages, leading to symptoms. - Axonal degeneration: This is when the neurons start to die off, also known as atrophy. Over time, the increasing brain volume loss can affect the entire brain or only a limited area or region. When atrophy happens in one location, the decrease of function is limited to that part of the brain. That said, atrophy development is the best predictor of future physical and cognitive disability, according to a
2019 review . - Remyelination: Your body tries to rebuild the myelin, but not always successfully.
- Scarring (sclerosis): Scarring develops on the damaged areas after severe flares of inflammation and degeneration.
It’s important to note that not every type of MS goes through all of these phases in the same way. Typically, the following occurs:
- Clinically isolated syndrome (CIS): Inflammation happens once and then resolves, which means that there tends to be less degeneration, atrophy, or sclerosis early in the disease.
- Relapsing-remitting multiple sclerosis (RRMS): You have periods of flares that then resolve, which also means that there tends to be less degeneration, atrophy, or sclerosis early in the disease.
- Primary progressive multiple sclerosis (PPMS) and secondary progressive multiple sclerosis (SPMS): Your symptoms develop gradually without a resolution due to degeneration and scarring.
When treating MS, the goal, especially with disease-modifying drugs, is to try and prevent episodes and relapses and minimize both scarring and atrophy.
Although there’s no cure for MS, many experts suggest cognitive rehabilitation, which includes behavioral interventions that focus on mental exercises or restorative interventions and compensatory strategies to improve cognition, according to a 2021 study review.
Restorative rehabilitation uses repetitive cognitive exercises to reinforce, strengthen, and recover cognitive skills. Meanwhile, compensatory strategies help people with MS learn ways to compensate for their cognitive difficulties by using tools like reminders and visualization.
Adjusting your lifestyle to encourage brain health can also be helpful. This can include:
- getting regular physical exercise
- maintaining a moderate weight
- engaging in activities that stimulate the brain like reading or doing puzzles
- limiting smoking and alcohol consumption
- taking all of your medications as prescribed
That said, it’s important to speak with your doctor to make sure that these or other changes are appropriate for you given your overall health and the progression of your symptoms.
Watch out when switching MS medications
Switching MS medications requires careful monitoring by you and your treatment team. Stopping disease-modifying medications without replacing them with a new one can lead to an increase in MS symptoms, including cognitive problems.
Also, compared with people who stay on their MS medications, you may have a higher hazard for disability progression, especially if you’re older, according to a
Dealing with the long-term effects of MS, including the impact it has on the brain, is trying and can often feel overwhelming. However, being in regular contact with your treatment team and having a support system in place can help.
If you have concerns about cognitive dysfunction or changes in moods or would like information on what you can do to address memory issues, talk with your doctor about the next steps. They can help refer you to any other healthcare professionals or recommend treatments that may provide relief.
