J-pouch surgery can successfully relieve symptoms of ulcerative colitis if medications and other treatments haven’t worked, but complications may arise.
Depending on the type of irritable bowel disease (IBD) you have, different surgeries remove different parts of the GI tract to prevent further damage. J-pouch surgery is one procedure used specifically for ulcerative colitis (UC).
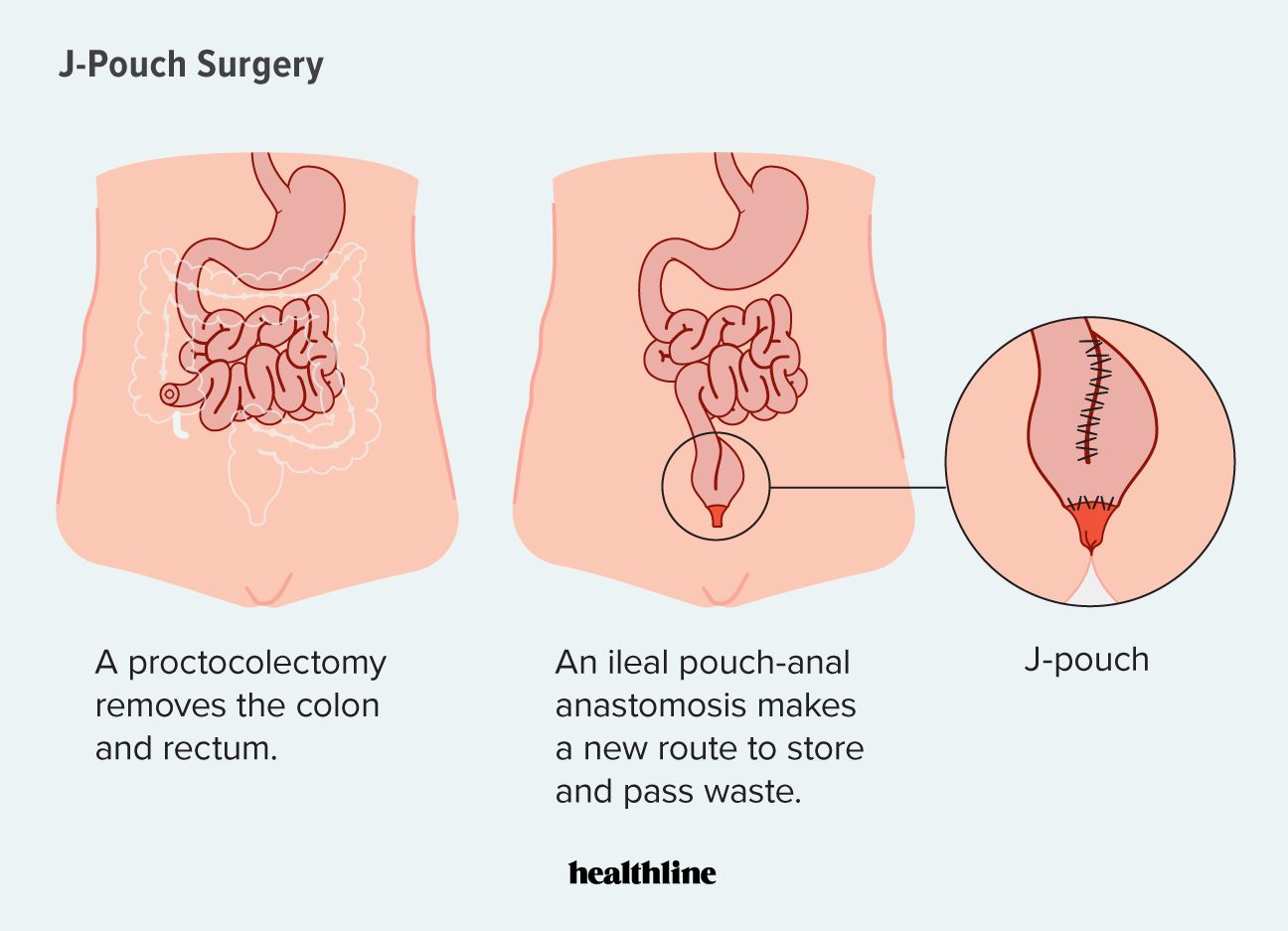
J-pouch surgery, also known as proctocolectomy with ileal pouch-anal anastomosis (IPAA), is a procedure used to treat severe ulcerative colitis (UC) and is considered the most common surgery for this condition.
Like other IBD surgeries, J-pouch surgery is only recommended in cases when medications for UC no longer work. The procedure may also be performed on an emergency basis for toxic megacolon or uncontrolled GI bleeding.
It involves a surgeon removing both the rectum and colon. They then take a portion of the small intestine and create a J-shaped pouch to collect and aid in waste removal.
You may be considered an ideal candidate for J-pouch surgery if you:
- currently experience UC symptoms
despite taking medicationsTrusted Source - notice your UC symptoms are worsening
- have precancerous colon cells
- are experiencing uncontrollable bleeding from your colon (a rare condition)
- have developed holes in your colon from chronic inflammation
- need surgery to remove your colon and rectum but would rather have an internal pouch to collect waste instead of an ostomy (external stool bag)
You may benefit from J-pouch surgery for UC if you have extensive damage spreading throughout your colon and rectum and if medications are not managing your symptoms.
After J-pouch surgery and recovery, you may experience fewer UC symptoms.
One advantage of J-pouch surgery compared with other procedures for UC is that the J-pouch itself eliminates the need for an external stool bag.
After full recovery, you won’t need to wear an ostomy or empty it, and you’ll have more natural control over your bowel movements.
Depending on how many stages your surgery is performed in, you may need to use an ostomy temporarily.
According to the Crohn’s & Colitis Foundation, J-pouch surgery for UC is typically performed in two stages, sometimes three, each scheduled several weeks apart.
First stage
- Your surgeon removes your rectum and colon.
- They take a portion of your small intestine known as the ileum and form it into a J-shape, or “J-pouch.”
- To allow time for the newly formed pouch to heal, your surgeon creates a temporary ileostomy (opening in the abdominal wall). A loop of your small intestine is pulled through this opening to form a stoma, so waste can exit your body into an ostomy bag.
Second stage
Your surgeon performs the second stage of this procedure about 2 to 3 months after the first stage.
- Your surgeon disconnects the ileum from the temporary ostomy.
- They reconnect the ileum of your small intestine to the J-pouch created from the first surgery.
- Once connected, your waste collects in the J-pouch, so you naturally pass stools through your anus.
Third stage (only used in certain cases)
Sometimes, a three-stage surgery is recommended. This involves an additional step where the J-pouch is directly connected to your anus.
This three-step process may be used in the following cases:
Why the procedure is done in stages
Rarely, J-pouch surgery is done completely in one procedure because the newly formed J-pouch needs time to heal to avoid infection.
According to the Crohn’s & Colitis Foundation, each stage of J-pouch surgery is performed 8 to 12 weeks apart.
If you have a temporary ostomy, you’ll need to follow your doctor’s care instructions for emptying it and keeping it clean.
You may experience an increase in bowel movements after your surgery, possibly up to 12 times in one day. Your number of daily bowel movements will gradually decrease after several months as your anal sphincter muscles grow stronger.
Your doctor may advise you to wait at least 6 weeks before resuming any physical activity. The exact timeline depends on how well your GI tract heals after surgery and if any complications arise.
The J-pouch procedure is considered a major surgery, so there’s a risk of infections, bleeding, and side effects from general anesthesia.
Sometimes, the newly formed J-pouch can become infected. This risk is higher in one-stage procedures. Other potential complications include:
- Small bowel obstruction: While considered uncommon with this surgery, temporary small bowel obstruction due to adhesions between tissues can occur. Bowel rest can treat it.
- Pouchitis: Inflammation and infection of the J-pouch occur in around half of those who undergo this surgery. While it’s treatable with antibiotics, you may experience fever, diarrhea, and abdominal pain.
- Pouch failure: If your body does not respond to the newly formed J-pouch, your surgeon may recommend a traditional stoma. In this case, the J-pouch will need to be surgically removed.
- Phantom rectum: A
common occurrenceTrusted Source after rectum removal, a phantom rectum may cause pain or feeling the need to pass stools, even without a rectum. Pain relievers, guided imagery, and antidepressants may be used for treatment. - Sexual dysfunction: Caused by nerve damage, it can occur in anyone.
- Infertility: In the female reproductive system, scar tissue that grows around both the fallopian tubes and ovaries can lead to fertility challenges.
The outlook for people who get J-pouch surgery is positive, with few experiencing pouch failure.
A 2022 review of 26 studies suggests pouch failure occurs in
Your doctor may recommend either an ostomy or another type of colorectal procedure called a K-pouch surgery if pouch failure occurs.
Pouchitis is the most common problem following J-pouch surgery and other pouch surgeries. It’s treatable and doesn’t mean you’ll develop pouch failure. Chronic pouchitis, however, has been linked to the possible failure of the J-pouch.
Your doctor may recommend J-pouch surgery if other treatment methods don’t provide relief for your ulcerative colitis (UC). It’s the most common surgery for UC and is sometimes used as an emergency surgery.
During J-pouch surgery, a surgeon removes your colon and rectum and uses your small intestine to create an internal pouch for waste collection. For some people, this method is preferred to wearing an external ostomy.
It’s important to discuss all the potential benefits and risks of a J-pouch procedure with your doctor. The outlook is positive, but complications may still arise.